In Brief
Applying a thoughtful note taking structure to your client sessions can help you stay as concise and focused as possible when documenting and planning a path forward. When remaining goal-oriented and responsive to client needs are at the center of your format selection, GIRP can be a great fit.
What are GIRP Notes?
GIRP notes are a structured method for documenting therapy sessions, focusing on four key components: client-centered Goals, therapist Interventions applied, your client’s observable Response, and setting an actionable Plan for next steps. GIRP notes provide a comprehensive snapshot of each session – facilitating continuity of care, supporting positive outcomes, and, of course, compliant documentation.
What separates GIRP notes from other options is that they place a strong emphasis on setting and tracking client-centered goals – this makes them particularly well-suited to goal-oriented therapy approaches, as well as meeting documentation standards set by insurance companies. When applied correctly, this note structure also supports effective treatment planning by clearly linking interventions to specific goals and tracking client progress over time, as well as enabling clear communication among other clinicians so that everyone is working towards the same objectives.

Benefits of GIRP Notes
With respect to focusing on goal-oriented therapeutic approaches, GIRP notes offer numerous advantages and considerations for therapists The benefits of using GIRP notes include:
- Enhances clarity and consistency: The structured format of GIRP notes ensures that session documentation is clear, organized, and consistent across all clients and sessions.
- Allows for measurable progress tracking: By focusing on specific, measurable goals, GIRP notes enable therapists to track client progress more effectively. This data-driven approach helps identify areas of improvement and adjust treatment plans accordingly.
- Supports collaborative care: GIRP notes promote effective communication and collaboration. It ensures that all mental health professionals involved in care are aligned with the client's goals and treatment plan, leading to more cohesive and coordinated care.
- Ensures comprehensive documentation: GIRP notes provide a comprehensive record of each therapy session, including your client’s’ goals, interventions used, client response, and future plans. This thorough documentation is essential for legal, insurance, and ethical purposes, as well as for continuity of care.
The goal-oriented nature of GIRP notes helps therapists develop targeted, personalized treatment plans that address each client's unique needs and objectives. This approach empowers clients to take an active role in their treatment, leading to increased engagement, motivation, and satisfaction with the therapeutic process.
How to Write GIRP Notes
Writing clear, concise GIRP notes involves capturing the essential elements of each therapy session within a structured, goal-oriented framework. Let’s break down those components:
Step 1: Goals
This area serves as the foundation of the GIRP approach, as it outlines the specific objectives the client aims to achieve. When writing this section, ensure that the goals are client-centric, are both short-term and long-term goals, and directly address your client’s presenting concerns. When setting goals, use the SMART criteria so that they’re clear and measurable for tracking progress over time.
Step 2: Intervention
Here, you’ll detail your contribution as the therapist in the session to support your client’s progress. This also includes noting the therapeutic techniques, strategies, and modalities you employed during the session. Be sure to add specifics of the therapeutic approaches you applied (e.g. cognitive behavioral techniques, mindful exercises) and demonstrate how those interventions directly support the client's goals and treatment plan.
Step 3: Response
Then, you’ll describe your client's reactions, insights, and progress in relation to your interventions. This will include things like examples of any shifts in your client’s affect, behavior, as well as your assessment of how well your client responded based on their engagement, and feedback. It will also include a sentence on any progress towards their goals.
Step 4: Plan
Last, this step is where you’ll outline future directions for therapy based on the session's outcomes. This will include setting actionable next steps, like homework assignments or exercises to complete between sessions; the therapist’s plan for interventions or approaches in future sessions, any scheduling of follow-up sessions, and any relevant referrals. Be specific and action-oriented in your planning, ensuring that the next steps towards client goals are clear and measurable.

When to Use GIRP Notes
GIRP notes are a versatile tool that can be applied across various therapeutic contexts, but they are particularly well-suited for:
- Goal-Focused Sessions: By documenting the client's goals, the interventions used, their response, and the plan for future sessions, GIRP notes provide a clear structure to track progress and refine interventions as needed.
- Long-Term Treatment Monitoring: For clients with established, ongoing treatment plans and long-term goals, GIRP notes offer a consistent method for documenting how interventions contribute to goal achievement over time.
- Behavioral Health and Skills-Based Interventions: The structured format of GIRP notes enables you to clearly link interventions to specific behavioral or cognitive goals, and track your client's development of new skills or behavior patterns.
- Progress Evaluation: When you need to evaluate your client’s progress or assess if interventions are effective, these notes are geared for documenting changes and refining treatment plans accordingly.
Using GIRP notes in scenarios like these allows for a goal-centered approach, with a clear framework for monitoring and measuring progress, whether your interventions need to be adjusted. That said, like any other format, consider what style of documentation aligns best with the goals of the session.
Examples of GIRP Notes
Depression Symptoms
- Goal: Reduce depressive symptoms as evidenced by client spending 2 hours outside of their bedroom with friends or family each evening after work.
- Intervention: Therapist utilized cognitive-behavioral therapy techniques to challenge negative thought patterns. Therapist encouraged client to engage in behavioral activation, including identifying daily BA goals to socialize with friends and family more and problem solving around barriers to meeting these goals.
- Response: Client reported a slight improvement in mood and increased engagement in pleasurable activities, such as listening to music and drawing. Client reported they met goal to spend time outside of their bedroom one night in the last week when they went on a walk with their mother. Client expressed hopefulness to go on a walk again this week as well as go to a movie with a friend.
- Plan: Continue exploring cognitive distortions and problem-solving barriers to meeting goals in next session in 1 week. Therapist assigned homework of keeping a thought journal.
Individual Session: Anxiety Disorder
- Goal: Client will reduce panic attacks from 3x/week to 0x/week.
- Intervention: Therapist provided client with safe space to check in and process experiences of the past week. Therapist iIntroduced relaxation techniques and facilitated Box Breathing exercise to support client in use of coping skills to manage panic attacks outside of session. Therapist provided psychoeducation on gradual exposure therapy. Discussed using this modality in future sessions to address panic triggers.
- Response: Client successfully practiced deep breathing exercises during the session and expressed willingness to confront feared situations. The client reported having 2 panic attacks in the past week, indicating some progress towards goal Client reported they were able to seek support from their partner to help them manage anxiety during both situations and they resolved fairly quickly.
- Plan: Therapist and client will develop a hierarchical exposure plan. Client given homework to schedule regular practice of relaxation techniques between sessions
Common Pitfalls in GIRP Note Writing
While GIRP notes provide a clear, goal-oriented framework for documentation, there are a few common mistakes to avoid:
- Failing to link interventions to goals: GIRP notes are most effective when each intervention directly supports the client's treatment goals. Not making that connection can make it difficult to track progress and assess the effectiveness of the therapy.
- Using vague or ambiguous progress language: In the Response section, aim to avoid using generic phrases like "the client seemed better" or "they made some progress." Instead, describe concrete changes, such as "the client reported a 20% reduction in anxiety symptoms" or "they successfully used deep breathing techniques to manage stress in a challenging situation."
- Overemphasizing interventions at the expense of progress: While it's important to document the interventions used, it's equally crucial to focus on the client's response and progress toward their goals.
- Failing to update the plan based on the client's response: If the client's response indicates that a particular intervention or goal isn't working, it's essential to adjust the plan accordingly.
By being mindful of these common pitfalls, therapists can maximize the effectiveness of your notes in supporting client goals, tracking progress, and ensuring high-quality documentation of your process.

GIRP Notes Compared to Other Formats
While all note taking formats serve the purpose of recording critical information, they differ in structure and emphasis. Here are a few ways that GIRP compares to other popular formats:
- SOAP (Subjective, Objective, Assessment, Plan): SOAP notes provide a comprehensive overview, including the client's self-reported experiences, therapist observations, clinical assessment, and treatment plan.
- DAP (Data, Assessment, Plan): DAP notes are more concise, focusing on the therapist's analysis and treatment plan based on collected data.
- BIRP (Behavior, Intervention, Response, Plan): BIRP notes emphasize the client's behavior and their response to interventions, making them useful for tracking consistent care across multiple providers.
- PIRP (Problem, Intervention, Response, Plan): PIRP notes center around identifying and addressing specific problems, documenting interventions, and monitoring the client's response.
Overall, GIRP notes are an excellent choice for those who want to maintain a strong focus on client goals and measurable outcomes, while other formats may be more appropriate for different clinical contexts or documentation needs. There’s no right or wrong choice for note formats – the key is to select a note type that enables clear, consistent, and comprehensive documentation so you can be most effective.
Frequently Asked Questions (FAQ)
Are GIRP notes HIPAA compliant?
They are when they are stored securely and kept separate from other client information. It's crucial to use a secure, encrypted platform for electronic documentation and to maintain client confidentiality.
How detailed should GIRP notes be?
Your GIRP notes should be comprehensive enough to capture the essential elements of each session, including goals, interventions, client responses, and plans. However, they should also be concise and focused on key points, avoiding unnecessary details that don't contribute to the therapeutic process.
Can GIRP notes be used for insurance purposes?
Absolutely – when writing GIRP notes for insurance documentation, it's important to demonstrate the client's progress and ongoing need for therapy, justifying the medical necessity of the sessions. Be sure that each note relates back to the client's diagnosis and treatment plan.
What additional resources are available for learning about GIRP notes?
Many professional organizations, such as the American Psychological Association and the National Association of Social Workers, offer guidelines and resources for effective documentation, including GIRP notes. It’s also worth considering continuing education courses and workshops, which can provide valuable insights and practical strategies for implementing GIRP notes in your practice.
Final Thoughts on GIRP Notes
GIRP notes are a powerful framework for your documentation, ensuring that the treatment you provide is goal-oriented, client-centered, and responsive to your client’s individual needs. Because of the information that is reflected in the format, the focus of these notes is around goals, which better sets you up for monitoring progress, effective treatment planning by providing a place to assess your interventions and if changes need to be made.

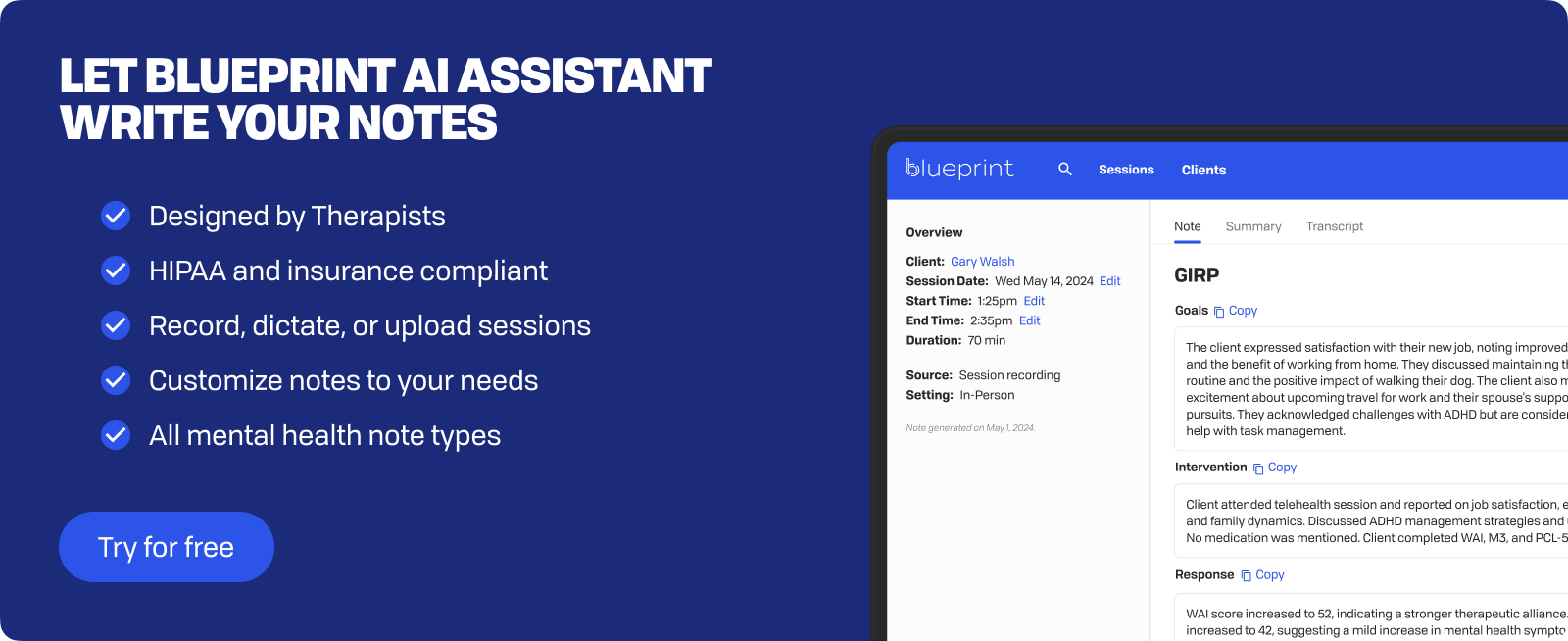
How Blueprint can help streamline your workflow
Blueprint is a HIPAA-compliant AI Assistant built with therapists, for the way therapists work. Trusted by over 50,000 clinicians, Blueprint automates progress notes, drafts smart treatment plans, and surfaces actionable insights before, during, and after every client session. That means saving about 5-10 hours each week — so you have more time to focus on what matters most to you.
Try your first five sessions of Blueprint for free. No credit card required, with a 60-day money-back guarantee.
























